Part 3 of 3: Refusing (Caregiving) Help: Why I Say No To "Help" – Sometimes
The Deposit Isn’t Refundable?
Summary: In the last part of my three-part series on Help, let’s talk about whether or not we accept the help available to us. Help has to be Helpful! See part one, Defining Help, and part two, Recognizing Help.
Written By: Trish Hughes Kreis exclusively for Assisted Living Directory

Why would we even consider refusing help?
Because help has to be helpful.
Let me explain.
There is a variety of help through government agencies and programs. Unfortunately, you practically need a Ph.D. in Bureaucracy in order to even know about this help, much less get it. I have cared for my disabled brother, Robert, for several years and am still learning what help is available butRefusing Caregiving Help do know that Medicare and Medicaid provide a great deal of specific help. Emphasis on specific.
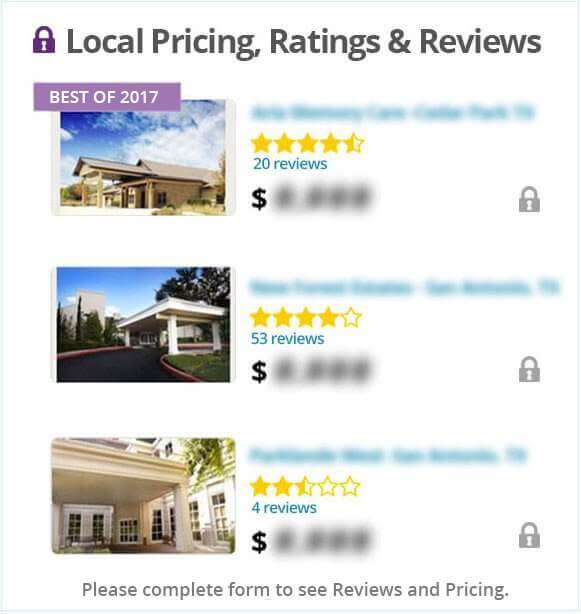
(As a side-note, this site, Assisted Living Directory, does a terrific job in outlining how to get some of this specific help geared toward financial assistance for living in an Assisted Living Facility.)
Help that may be helpful but not easily known takes persistence, the willingness to ask questions and a love of solving puzzles. Following are a few tips to find help that is actually helpful:
1. Enlist the help of the doctor’s staff. Robert is now able to get non-generic anti-seizure medications because his neurologist determined these were medically necessary. It took a little back and forth between the doctor’s office staff and Medicare but the medications were finally approved for payment. I was grateful to the doctor’s office for their help and gladly accepted their help.
2. Recognize when help is not available. Remarkably, Robert is not able to get Medicare or Medicaid to pay for his helmet no matter how medically necessary it is. We pay for that out of pocket but it is quite startling to me that this piece of medical equipment is not paid for when head injuries due to seizures (and occurring before Robert wore a helmet) are now causing a great deal of health problems for Robert. Health problems resulting in medical expenses which are covered under Medicare and Medicaid. Nothing makes my blood boil more than the illogical and arbitrary rules of Medicare and Medicaid and other government programs! The medical supply company that fits Robert for his helmet finally shared with me (after two rounds of ordering helmets) that the helmet was not covered. The company had been paying for it out of their pocket because they hadnt advised me of the cost before ordering. Now that is a company (Hanger Prosthetics) with integrity that I will continue to use and recommend.
3. Ask questions. Then ask a few more. Robert’s hospitalizations are covered by Medicare and Medicaid. A stay in a Skilled Nursing Facility is also covered although it has to be immediately preceded by a hospital stay. Generally, 100 days are covered in a SNF per incident (there are specific rules regarding the 100 days and what constitutes a separate incident). I did not know this until I asked questions about the rules and looked on the Medicare website.
4. Discharge Help. Not all hospital discharge coordinators are created equal. After a hospitalization or a stay in a SNF, home physical therapy and nursing care is covered for an undetermined amount of time. (It’s difficult to get an exact answer to this question as it seems the home health care service has some flexibility depending on the progress of the patient.) Not all discharge coordinators make caregivers aware of this benefit. If nothing is mentioned during the discharge process, please ask about it. This is the sort of help that can be extremely beneficial upon release from the hospital.
5. Consider Options. Oddly enough, there is not an option to choose outpatient physical therapy instead of home physical therapy after a discharge from a SNF or hospital stay. I wanted Robert to continue his physical therapy at the SNF where he had made great progress. This would be more helpful to him than starting with a new therapist in our home so I again enlisted the help of his neurologist to write a prescription for outpatient physical therapy. It was more time-consuming for me as the caregiver to choose this option but it was more helpful to Robert.
There is an abundance of help I will happily accept. There is help that I need to dig to find (or recognize) and help that I choose to reject.
Each caregiving situation is different but once help is defined and recognized by the caregiver, more help may arrive (or have already been present). Once that happens we can accept that help, see it as help or say thank you but no thank you to the help.
It is empowering to know we have choices when it comes to our help.
See the first part of this series is on defining help
See the second part of this series is on recognizing help.
Article by Trish Hughes Kreis exclusively for Assisted Living Directory
Comming Soon:
No Obligation
Assisted Living with Part 3 of 3: Refusing (Caregiving) Help: Why I Say No To "Help" – Sometimes